MY Comment, by KEN GRAUER, MD (6/16/2025):
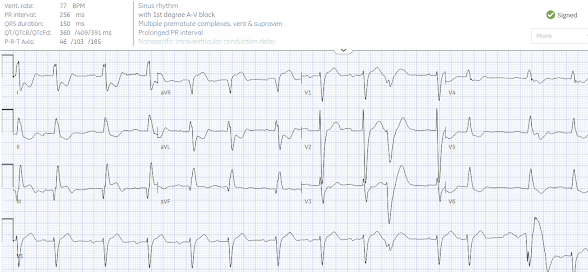
- For clarity in Figure-1 — I've reproduced and labeled this repeat ECG.
- Caveat: As per Dr. McClaren — the KEY clue for suggesting that the WCT in today's 1st ECG was supraventricular, was the fast septal depolarization (ie, narrow initial R wave in leads V1-to-V3). That said — I'll add the caveat that as helpful as this clue is, it is not infallible — as I've seen documented VT on occasion manifest surprisingly narrow initial QRS deflections in these anterior leads. The reason I was not confident in today's case about a supraventricular etiology for the WCT until I saw ECG #2 — was that the initial QRS deflection in the WCT rhythm was wide in many of the other leads.
- But the presence of sinus P waves with a constant (albeit prolonged) PR interval in the long lead V1 rhythm strip (RED arrows) — confirmed the supraventricular etiology in Figure-1.
- While fully acknowledging that additional details regarding the rhythm in Figure-1 do not alter management — facile use of the long lead V1 rhythm strip in association with the simultaneously-recorded leads from the 12-lead tracing above it, allow clarification that the PINK arrow P waves in Figure-1 are PACs — because: i) Beats #2,6 and 12 all occur earlier-than-expected; ii) The PR interval of these 3 beats is consistently shorter than the PR interval of the RED arrow P waves; and, iii) P wave morphology of the 4 PINK arrow P waves in Figure-1 is subtly different than the P wave morphology of the RED arrow sinus P waves (these PINK arrow P waves all lack the terminal negative P wave deflection of the sinus P waves).
- In contrast — beat #10 is a PVC, even though the QRS complex of this beat is small in the long lead V1 rhythm strip. We know this — because simultaneously-recorded beat #10 in leads V1,V2,V3 is clearly very wide and very different in morphology compared to beats #8,9 and 11 in these leads.
- However — beat #13 in the long lead V1 rhythm strip is not a PVC. We know this despite how wide and different-looking this beat is in lead V1 — because the QRS morphology of beat #13 in simultaneously-recorded beat #13 in leads V4,V5,V6 is identical to the QRS morphology of beats #12 and 14 in these leads. It should be apparent that the reason for the bizarre QRS morphology of beat #13 in the long lead V1 is the result of artifact.
- "Take-Home" — In my experience, the concept of assessing P wave and QRS morphology using simultaneously-recorded leads is underused. While not clinically important in ECG #2 — there are times when this technique will be the sole determining factor for distinguishing between an SVT vs VT.
- As discussed by Dr. Meyers and in My Comment from the December 31, 2024 post of Dr.Smith's ECG Blog — the combination of ST elevation in lead III (but not in other inferior leads) — in association with an ECG picture that is otherwise consistent with DSI (Diffuse Subendocardial Ischemia) — suggests there is inferior OMI plus underlying multivessel disease.
- The diagnosis of DSI in today's case is suggested by ST depression in multiple leads (as per the 7 BLUE arrows in Figure-1) — in association with marked ST elevation in lead aVR.
- Although we are only provided with information from the cardiac catheterization report regarding the "culprit" LCx artery — the bizarre IVCD morphology, in association with fragmented QRS complexes in several leads is almost certain indication of additional underlying "scar" from coronary disease.
Written by Jesse McLaren
A 65 year old with history of CABG and end stage renal disease developed sudden chest pain and diaphoresis during routine dialysis, and was given three nitro sprays and then sent to the emergency department. On arrival, heart rate was 145 and BP 75/50. What do you think?
There’s a wide complex tachycardia which is regular (so not AF) and without preceding P waves (so not sinus tach). There’s a LBBB appearance in the precordial leads, but the limb leads have rS complexes in I/aVL rather than monophasic R waves – making it non-specific intraventricular conduction delay (IVCD). There are no obvious features of hyperkalemia (eg very wide QRS, peaked T waves). Instead, There’s fast septal depolarization in V1-3 (narrow rS) suggesting supraventricular origin. With the abnormal depolarization there's expected discordant repolarization abnormalities, which are exaggerated by the tachy-arrhythmia - producing diffuse ST depression with reciprocal STE in aVR. But there's unexpected concordant STE in III, which could be secondary to the tachy-arrhythmia or from primary ischemia. Bottom line: unstable non-sinus tachy-arrhythmia: cardiovert and reassess.
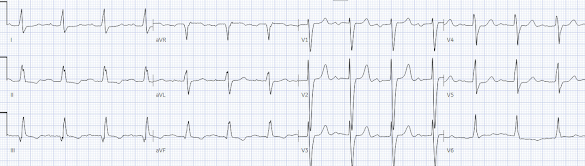
The patient spontaneously cardioverted and systolic BP increased to the 90s, but had ongoing chest pain. Repeat ECG:
Sinus rhythm with PVC, first degree AV block, and same QRS morphology as during tachy-arrhythmia - confirming it was supraventricular. The final blinded read was non-specific IVCD, suggesting that all ST/T changes are secondary to abnormal depolarization. But there is still ongoing inappropriate concordant ST elevation III and reciprocal ST depression I/aVL, as well as mild concordant ST depression in V2 - indicating superimposed primary ischemic changes from inferior +/- posterior OMI.
Old MI can result in Q waves with residual STE (LV aneurysm morphology), which in the inferior leads can be difficulty to distinguish from acute OMI. But this was new compared to an old ECG:
The old ECG also had a narrower QRS, so cath lab was activated both for “new LBBB” as well as concordant inferior ST elevation. But it’s not a true LBBB, and “new LBBB” is no longer an indication for cath lab activation. However, despite not being a true LBBB, the principle of inappropriate concordance is still helpful in identifying OMI.
Even without a prior to compare, this ECG in a patient with a high pre-test likelihood of ACS is diagnostic of OMI. Here's the Queen's interpretation, highlighting concordant STE and reciprocal STD:
What about the initial troponin? Troponin is often chronically elevated in a dialysis patients, and can rise from the demand ischemia of tachy-arrhythmias or other shock states. The initial troponin is an unreliable marker of acute OMI (it can be normal acutely, and even if elevated it lags far behind the myocardial damage), and doesn’t provide real-time information to distinguish Occlusion MI from Non-Occlusion MI. So in this patient the initial troponin would not help differentiate chronic myocardial injury, type 2 MI from tachy-arrhythmia demand ischemia, and type 1 MI from OMI or NOMI – and if OMI, waiting for troponin would cost myocardium. So this is a clinical diagnosis, aided by ECG.
Fortunately the patient was immediately taken to cath lab without waiting for the troponin, with a door to cath time of only 45 minutes. There was a 95% left circumflex occlusion which was stented. First troponin I was 80 ng/L (only slightly higher than the patient’s baseline of 50ng/L), which rose to 500, then 2,000 and then a peak of 8,000 ng/L. Follow up ECG showed resolution of the primary ischemic ST changes, and subtle infero-posterior reperfusion T wave inversion compared with baseline:
Take home
1. If a patient is unstable from a WCT and the differential is narrowed to VT vs SVT with aberrancy (eg not AF, sinus tach, or hyperkalemia/sodium channel toxicity), then the treatment is immediate cardioversion regardless
2. Tachy-arrhythmias can cause secondary ST/T changes that can be reassessed after cardioversion
3. ‘New LBBB’ is not an indication for cath lab activation
4. Inappropriate concordant STE can identify OMI in both LBBB and IVCD
5. First troponin is an unreliable marker of OMI in acute chest pain and can’t differentiate chronic myocardial injury and demand ischemia from OMI or NOMI: OMI is a clinical diagnosis, aided by ECG (and AI)
MY Comment, by KEN GRAUER, MD (6/16/2025):
- For clarity in Figure-1 — I've reproduced and labeled this repeat ECG.
- Caveat: As per Dr. McClaren — the KEY clue for suggesting that the WCT in today's 1st ECG was supraventricular, was the fast septal depolarization (ie, narrow initial R wave in leads V1-to-V3). That said — I'll add the caveat that as helpful as this clue is, it is not infallible — as I've seen documented VT on occasion manifest surprisingly narrow initial QRS deflections in these anterior leads. The reason I was not confident in today's case about a supraventricular etiology for the WCT until I saw ECG #2 — was that the initial QRS deflection in the WCT rhythm was wide in many of the other leads.
- But the presence of sinus P waves with a constant (albeit prolonged) PR interval in the long lead V1 rhythm strip (RED arrows) — confirmed the supraventricular etiology in Figure-1.
- While fully acknowledging that additional details regarding the rhythm in Figure-1 do not alter management — facile use of the long lead V1 rhythm strip in association with the simultaneously-recorded leads from the 12-lead tracing above it, allow clarification that the PINK arrow P waves in Figure-1 are PACs — because: i) Beats #2,6 and 12 all occur earlier-than-expected; ii) The PR interval of these 3 beats is consistently shorter than the PR interval of the RED arrow P waves; and, iii) P wave morphology of the 4 PINK arrow P waves in Figure-1 is subtly different than the P wave morphology of the RED arrow sinus P waves (these PINK arrow P waves all lack the terminal negative P wave deflection of the sinus P waves).
- In contrast — beat #10 is a PVC, even though the QRS complex of this beat is small in the long lead V1 rhythm strip. We know this — because simultaneously-recorded beat #10 in leads V1,V2,V3 is clearly very wide and very different in morphology compared to beats #8,9 and 11 in these leads.
- However — beat #13 in the long lead V1 rhythm strip is not a PVC. We know this despite how wide and different-looking this beat is in lead V1 — because the QRS morphology of beat #13 in simultaneously-recorded beat #13 in leads V4,V5,V6 is identical to the QRS morphology of beats #12 and 14 in these leads. It should be apparent that the reason for the bizarre QRS morphology of beat #13 in the long lead V1 is the result of artifact.
- "Take-Home" — In my experience, the concept of assessing P wave and QRS morphology using simultaneously-recorded leads is underused. While not clinically important in ECG #2 — there are times when this technique will be the sole determining factor for distinguishing between an SVT vs VT.
- As discussed by Dr. Meyers and in My Comment from the December 31, 2024 post of Dr.Smith's ECG Blog — the combination of ST elevation in lead III (but not in other inferior leads) — in association with an ECG picture that is otherwise consistent with DSI (Diffuse Subendocardial Ischemia) — suggests there is inferior OMI plus underlying multivessel disease.
- The diagnosis of DSI in today's case is suggested by ST depression in multiple leads (as per the 7 BLUE arrows in Figure-1) — in association with marked ST elevation in lead aVR.
- Although we are only provided with information from the cardiac catheterization report regarding the "culprit" LCx artery — the bizarre IVCD morphology, in association with fragmented QRS complexes in several leads is almost certain indication of additional underlying "scar" from coronary disease.
-USE.png)



No comments:
Post a Comment