MY Comment, by KEN GRAUER, MD (6/10/2025):
- XXXX
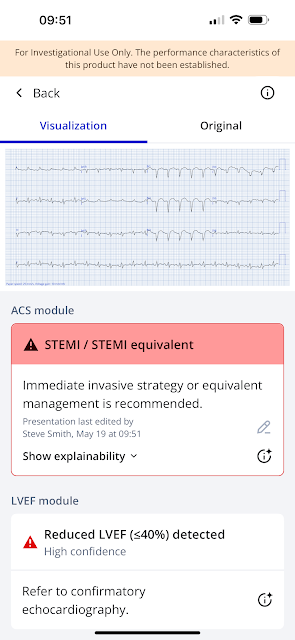
| Figure-1: The initial ECG in today's case. (To improve visualization — I've digitized the original ECG using PMcardio). |
5881888
Recent chest surgery. Had been to surgeon's office complaining of chest pain. Assumed to be post-surgical.
SOB with pulmonary edema.
acute hypoxic resp failure with "severe pressure on chest" put on BiPAP
she is concerned about an increase in fluid accumulation, as she is experiencing chest pain and shortness of breath. A few days ago, she had some shortness of breath, but her surgeon was not concerned at that time. However, today she describes a sensation of "an elephant sitting on her chest."
Cardiac ultrasound showed a possible decreased function, IVC without respiratory variation, and B-lines at the lung bases bilaterally. Patient's troponin returned significantly elevated at 10,216.
Patient having significant increased work of breathing and given B-lines on cardiac ultrasound, she was started on BiPAP for respiratory support.
36 year-old who presents with chest pain. She underwent surgery to her chest three weeks ago on her chest, breast reduction, now she is concerned about an increase in fluid accumulation as she is experiencing chest pain and shortness of breath a few days ago, she had shortness of breath and surgeon was not concerned. However, today she describes feeling of an elephant sitting on her chest. She has significant family history of cardiac issues. Her first troponin was 10,216 and Rose to 10,655 and then dropped five hours later to 7459.
Here is the PMCardio AI ECG Model's diagnosis:
Notice that she also tells us that the Ejection Fraction (LVEF) is less than 40%. This is another great feature of this model.Abstract 4141318: AI-Powered Smartphone Application for Detection of Left Ventricular Systolic Dysfunction using 12-Lead ECG
Here is the troponin profile over 60 hours (most recent on the left, initial on the right):
Cardiac MRI
Dilated left ventricular size with moderately reduced left ventricular
systolic function, calculated EF 38%.
Prolonged native T1, T2, ECV without LGE suggests myocardial edema +
inflammatory cardiomyopathy without fibrosis.
Diffuse pericardial enhancement noted, consider pericarditis.
Discussion:
Patient is a 36 year old with a history of hypothyroidism and recent bilateral breast reduction who was admitted to the MICU for acute hypoxic respiratory failure with acute pulmonary edema and new reduced EF30%. Her respiratory failure has improved with diuresis.
CMRI is consistent with myopericarditis. Etiology is unknown at this point. Viral workup was negative, but need to pursue additional workup for her severe acute inflammatory myopericarditis. Starting valsartan for afterload reduction and will titrate. Continue telemetry and possible limited TTE to follow up LV function appropriate in 4 - 6 days or sooner with unexplained change in clinical status. Pain control appears to be improving. Continue present pain management.
Recommendations:
- 1. Acute hypoxic respiratory failure, improving, secondary to myocarditis
- a. Continue to manage pulmonary edema and other causes of respiratory failure
- b. Continue diuresis with IV lasix
- i. Active diuresis until patient is off O2 and is comfortable - would attempt to estimate volume status and verify patient is no longer clinically hypervolemic)
- ii. Monitor with BMP for renal function and contraction alkalosis
- c. Continuous telemetry, strict Is/Os, daily weights
- 2. Acute inflammatory myopericarditis
- a. Etiology: Recommend autoimmune/additional laboratory (HIV, ANA, autoimmune, etc) evaluation
- b. Rheumatological evaluation consultation to exclude autoimmune conditions
- c. cardiomyopathy/afterload: Start valsartan 20 mg BID
- d. Close monitoring on telemetry for arrhythmias
- e. Pain: Continue NSAID's and colchicine
- i. Additional pain management per primary
echo:
Moderately decreased left ventricular systolic function with an estimated
EF of 30%.
Diffuse hypokinesis of the mid and apical segments.
echo 9 days later:
LV systolic dysfunction.
The estimated left ventricular ejection fraction is 40 %.
No regional left ventricular wall motion abnormality.
Normal right ventricular size and function.




No comments:
Post a Comment