MY Comment, by KEN GRAUER, MD (6/14/2025):
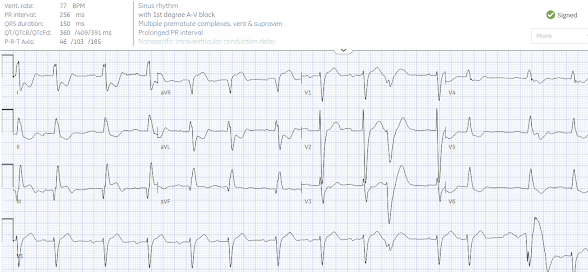
- Regardless of whether or not STEMI criteria were met — the important point is to recognize that today's initial ECG is clearly diagnostic of acute proximal LAD OMI.
- As per Dr. Smith — nearly all the benefit of reperfusion is lost by 6 hours. It is for this reason that cases such as the one presented today by Drs. Sala and Villa should be recognized within seconds of seeing an initial ECG like the tracing shown in Figure-1.
- Rapid recognition begins with the history. Knowing the patient is a 60-something man with known diabetes and COPD (therefore presumably a longterm smoker) — who presented with 1 hour of "oppressive" CP (Chest Pain) — instantly places this patient in a higher-risk group for having an acute cardiac event (ie, Our "threshold" for activating the cath lab should be lowered — so as to include not only diagnostic ECG findings, but also those ECG findings that are somewhat less certain, but still suspicious for OMI).
- Overall QRS amplitude is reduced, especially in the chest leads where none of the 6 leads manifests an amplitude greater than 7 mm. Whether this overall reduction in QRS amplitude is the result of body habitus, the patient's COPD — and/or reduced QRS amplitude as a result of cardiac stunning in association with acute infarction, is uncertain from this single tracing.
- Transition occurs surprisingly early (ie, The QRS becomes all positive as soon as in lead V2). The reason (and potential significance) of this unusual finding is uncertain — but important to appreciate in our assessment of ST-T wave appearance in anterior leads.
- The above said — my "eye" was immediately drawn to the ST-T waves in leads V2 and V3 (within the RED rectangle). That the T waves in both of these leads are hyperacute — should be recognized by the disproportionately enlarged T wave dimensions compared to the tiny QRS amplitudes in V2,V3.
- As noted by Dr. Smith — both leads V2 and V3 manifest T-QRS-D (Terminal QRS Distortion), because neither lead has a J-point or an S wave that descends below the baseline (See My Comment in the November 14, 2019 post in Dr. Smith's ECG Blog for more on T-QRS-D).
- In the context of the above described definitely abnormal ST-T waves in leads V2,V3 — Neighboring leads V1 and V4 are also clearly abnormal. The slight ST elevation with ST segment straightening, disproportionately prominent postive T wave with subtle terminal T wave negativity in lead V1 — is not normal for the ST-T wave appearance in this lead.
- By itself — I might not interpret the T wave in lead V4 as hyperacute. But in the context of definite hyperacuity with T-QRS-D in leads V2,V3 — the T wave in V4 is surprisingly tall, and both "fatter"-at-its-peak and wider-at-its-base than expected given modest R wave amplitude in this lead.
- Reciprocal changes are seen in each of the inferior leads. Light BLUE arrows highlight ST segment flattening in leads II,III,aVF — with slight ST depression in III and aVF — and (as emphasized by Dr. Smith), with telltale terminal T wave positivity (darker BLUE arrows) that supports an ongoing acute cardiac event.
- Finally — Lead aVL provides an excellent example of subtlety that by itself would not be significant — but which in the context of acute anterior chest lead findings + reciprocal ST-T wave changes in all inferior leads — confirms an acute event. That is, the shape of the ST-T wave in lead aVL is coved and ever-so-slightly elevated.
- PEARL: A proximal LAD location is suggested for this OMI because: i) An acute ST-T wave appearance begins with lead V1; ii) There are reciprocal ST-T wave changes in the inferior leads; and, iii) Lead aVL shows slight-but-real ST segment coving with ever-so-slight ST elevation.
-USE.png) |
| Figure-1: I've labeled today's initial ECG. |
This case came from Drs. Luca Sala and Paolo Villa from a public hospital (Ospedale Luigi Sacco) in Milan Italy.
CASE
A 60-something male presented with one hour of "oppressive" chest pain radiating to the back and to the left arm. He has a history of diabetes and COPD.
This ECG was recorded:
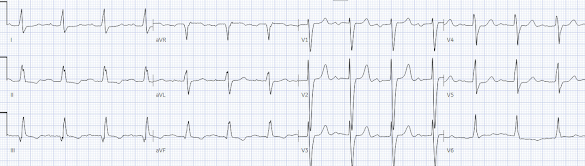
Here is the ECG after the PCI (digitized by PMCardio):
And the next day:





-USE.png)




-USE.png)

