-USE.png) |
| Figure-1: The initial ECG in today's case. (To improve visualization — I've digitized the original ECG using PMcardio). |
- Your tracings are too dark. I lightened them all for you and added a border. Feel free to use my version if you like. I will send you copies of my lightened versions. Be SURE to always make an EXTRA COPY of all originals — in case whatever labels you add turn out not to be what you want ...
- ECGs should be labeled either on the actual ECG — or in the legend. You'll note that I added (in RED) below each Figure — naming them ECG #1, #2, #3 for clarity. Otherwise it gets CONFUSING as to which tracing is which.
- I know you are interested in arrhythmias — which is great (You have some wonderful cases!) But IF you start delving into the world of complex arrhythmias — in my opinion you NEED to: i) Number all beats. Life is too short to have to count the beat number each time you make a comment; and ii) Start using either a "Markup" program (to add lines, arrows, numbers) or do this on Power Point. I use both — depending on what I am doing. Retrograde atrial activity here is subtle — so ARROWS at least for the first couple of examples of any given concept in my opinion are ESSENTIAL. Otherwise you'll quickly LOSE your readers (You've seen the way I do this — but you should develop YOUR own style. I suggested with similar feedback to Willy on his cath films illustrations — and he quickly developed his own wonderful style of labeling his illustrations. You should do the same. Find YOUR styling — and have fun "playing" with it!).
- Use BULLETS when explaining tracings. It gets jumbled (and confusing) when you put each rhythm finding in the same long paragraph ... PUT YOURSELF in the MINDSET of the READER! Imagine the reader who is very experienced with complex arrhythmia interpretation as well as the less experienced reader. ASK YOURSELF if your text address both types of readers — :)
- I think it is more effective (and pleasing to the eye) when asking key Questions (ie, How would you interpret the below tracing? ) — if you take out the underline and instead, use either bold or a new bullet for your questions ....
- Note that I took out the ? in ECG #3 — because your ? was too big ... Feel free to re-add a somewhat smaller question mark.
- I will eventually write a Comment — but at this point, I have NO IDEA of what I will write — so BEST not to say anything about my analysis (because I probably will choose not to comment on various aspects of this case). You can always add reference to my Comment after I write it if you like.
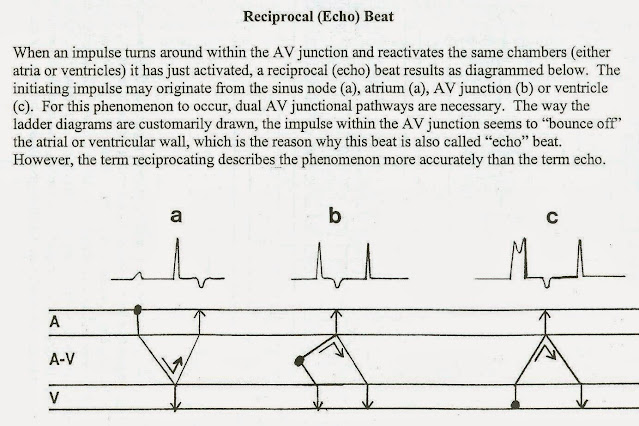
- Where did you get the last figure on the Reciprocal (Echo) Beat? I know I did not write this. Whenever you copy anything written by someone else — it is essential to cite where you got it from. I also often add LINKS if relevant. I generally cite this in the Figure legend and/or in the text and/or sometimes in both places.
- I still think your text would look much better if you JUSTIFY the margins (You'll note that all of my text is justified with an even right-sided margin).
The patient in today's case is a 70 something male who presented with a three week history of asthenia and intermittent palpitations. There was no chest pain, but he did describe shortness of breath on exertion and had a markedly reduced physical capacity. There was no syncope. Physical exam was unremarkable except radial pulse deficit. Chest X-ray normal. The patient had a coronary angiogram done 5 years prior which was completely normal. The patient was admitted for telemetry monitoring.
Below is a rhythm strip. How would you interpret the below tracing?
.png) |
| ECG #1 |
- When teaching arrhythmia interpretation — I emphasize that an amazingly simple thing to do that is INVALUABLE in facilitating interpretation (and in explaining what you are doing to others) — is simply to label all P waves in the tracing! I would do this here (using fairly small arrows that are not bigger than 1 large box in size). I generally use RED for obvious sinus P waves — and then I change colors depending on the point I am trying to illustrate. This makes it EASY to describe something by a colored arrow in seconds (ie, Note Willy's use of colored arrows in his cath film illustrations).
- The above paragraph is hard to read. Using bullets for each new descriptive point would go a LONG way toward simplifying.

.png) |
| ECG #3 |
In this tracing again there are PVCs in bigeminy with variable RP' interval. Given how much artifact the top 2 leads have — would be best to add colored arrows showing retrograde P waves ... Beat #9 is marked with a red question mark. This beat has a different morphology than the other wide complexes. What might account for the timing of this QRS complex and why does is appear different morphologically from the PVCs? NOTE — I think it best when asking questions to leave a bit MORE space before you give the answer! (Otherwise readers might unknowingly see the answer before they have a chance to formulate their response ... )
Answer: Beat number #9 is very likely an echo beat. (For detailed explanation see in depth analysis by dr Grauer below). Look at the preceding beat (#8, the PVC). That beat has retrograde capture of the atria with a long RP' interval. The electrical impulse after having traversed the AV node and activated the atria, then «echoes» back down the AV node (antegrade conduction) and captures the ventricles again (Beat # 9), now with LBBB morphology. now with aberrant conduction. The LBBB is due to the left bundle still being refractory. (Rate dependent LBBB) The only lateral lead you show on the rhythm strip of ECG #3 is lead V5 — but since the QRS is not all positive in V5 — we do not know if this is truly "LBBB aberration". I would not call it "rate-related BBB" — because we only see 1 beat, which is an Echo beat — and not a speeding up of the rhythm that favors rate-related aberrancy. True, the reason for the wide QRS may be similar to "rate-related aberrancy" — but I would simply say something like the different QRS morphology of beat #9 with its short coupling interval results in aberrant conduction.
As I mentioned above — important to add the specific source from where you are copying the Reciprocal (Echo) Beat figure ... And if you do use this figure — would be best to indicate that what happens is similar to "c" in this Figure, with the exception that the echo beat is aberrantly conducted.
Discussion: This patient was experiencing palpitations due to short runs av ventricular tachycardia. Asthenia was caused by pulseless ventricular premature complexes. Telemetry revealed dual AV pathway and echo beats. Stress test was performed, and the PVCs disappeared during exercise. Echocardiography revealed normal ventricular function and a structurally normal heart. An ICD/pacemaker was placed. The patient was started on betablocker therapy and discharged home. Follow up is unavailable.
- HOW do you know what is causing the palpitations? It could be the VT — but studies show that almost ANY RHYTHM ABNORMALITY may be the cause of palpitations (a point I would always include during my lectures on palpitations). Bradycardia may cause palpitations and so can single PVCs.
- Is Asthenia "caused" by pulseless PVCs? — or is it the persistent BRADYCARDIA that is more probably responsible for this patient's profound fatigue?
- I do think use of dual AV nodal pathways IS a possibility — but I don't think this is "revealed" by telemetry. (instead — the above rhythms strips suggest that dual AV nodal pathways may be operative).
- Your discussion sounds like Echo beats were common. Were they? Regardless if common or not — I think of Echo beats as more of an interesting phenomenon to make readers aware of — but not really something of clinical significance (as is implied here).
- Blood tests? (ie, Hct, electrolytes?)
- What did a 24-hour Holter monitor show ????? This patient is 70. Isn't SSS (Sick Sinus Syndrome) likely? Why are there PVCs and runs of VT? We may never find out for certain — but given a structurally normal heart — could it be that SSS with bradycardia is a fundamental problem, with inadequate oxygenation leading to ventricular ectopy?
- AGAIN — I ask lots of questions — but from what I read, I think lots of questions remain. That said — permanent pacing will probably cure this. The ß-blocker may or may not be needed — but no problem empirically using it since the pacer guarantees an adequate heart rate.
- YOU can "mold" your Discussion in ANY way you like — but I think would be good to make sure the story touches all bases. (And it is FINE to indicate that our data base on this patient is incomplete for answers to the questions I ask that are not known ... )

.png)

No comments:
Post a Comment