- XXXXX
-USE.png) |
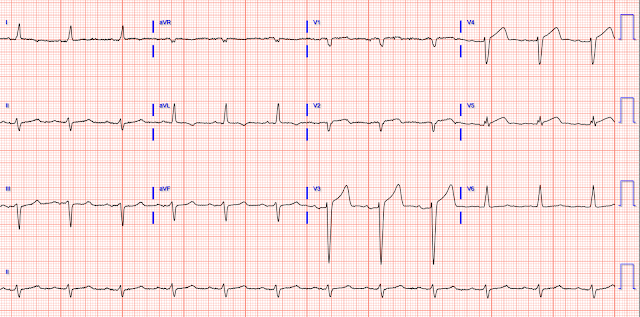
| Figure-1: Comparison between the initial ECG in today's case — and a prior baseline tracing on trial. Is there any acute change? |
-USE.png) |
| Figure-1: The initial ECG in today's case. (To improve visualization — I've digitized the original ECG using PMcardio). |
Sent by Anonymous, written by Pendell Meyers
Sent by Anonymous, written by Pendell Meyers
A man in his 60s with history of CAD and 2 prior stents presented to the ED complaining of acute heavy substernal chest pain that began while eating breakfast about an hour ago, and had been persistent since then, despite EMS administering aspirin and nitroglycerin. There was associated diaphoresis, but no dyspnea, nausea, vomiting. He reported having covid 2 weeks ago, but had seemingly fully recovered.
Triage 1104:
The ECG was interpreted correctly as "No STEMI." Due to the state of the ED at the time, the patient was placed in a waiting area.
Two prior / baseline ECGs on file:
The first high sensitivity troponin I returned elevated (upper limit of normal for men in this assay is 20 ng/L) at 25 ng/L. Unfortunately, the only action that was taken at this time was to repeat the troponin (still waiting in waiting area due to miserable boarding and overcrowding problems).
It is easy to say this in retrospect, especially not being the one in charge of this overcrowded waiting room full of unseen patients, but an elderly patient with known CAD and ongoing ACS-sounding chest pain with positive troponin is already an indication for emergent cath, regardless of the ECG!
The second troponin returned higher at 45 ng/L. This finally prompted a repeat ECG at 1341:
Formal echo showed EF 20% (previous EF on file 34% 5 months ago), severe global hypokinesis, akinesis of the mid-apical myoardium, akinesis of inferolateral, inferior, and inferoseptal myocardium.
He survived to discharge. Long term follow up not available.












No comments:
Post a Comment