- In addition to ST elevation in lead aVR — a lesser amount of ST elevation may also be seen in lead V1 with diffuse subendocardial ischemia (and sometimes also — as occurs in today's case, some ST elevation in lead aVL).
- The relative amount of ST elevation in lead aVR with diffuse subendocardial ischemia — tends to be comparable to the amount of ST depression seen in many of the leads.
- ST depression will not always be present in 9/12 leads — as is seen in Figure-1. Instead, diffuse subendocardial ischemia may be present with ST depression in only 7 leads.
- Finally — It is well to remember that the amount of ST segment deviation in ECG #1 is extreme! Much of the time — the amount of ST depression (and the amount of reciprocal ST elevation in lead aVR) will not be nearly as marked.
- Severe Coronary Disease (due to LMain, proximal LAD, and/or severe 2- or 3-vessel disease) — which in the right clinical context may indicate ACS (Acute Coronary Syndrome).
- Subendocardial Ischemia from another Cause (ie, sustained tachycardia — sinus or from some other arrhythmia; shock/profound hypotension; GI bleeding; anemia; etc.).
-USE.png) |
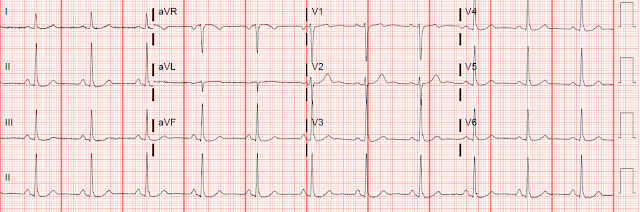
| Figure-1: The initial ECG in today's case. (To improve visualization — I've digitized the original ECG using PMcardio). |
- BOTTOM Line: The "good news" — is that health care providers in today's case promptly recognized the ECG picture as indication of diffuse subendocardial ischemia (and not of acute MI). And, after resolution of the acute allergic reaction — underlying coronary disease was appropriately ruled out before discharge.
-USE.png) |
| Figure-1: The initial ECG in today's case. (To improve visualization — I've digitized the original ECG using PMcardio). |
- Severe Coronary Disease (due to LMain, proximal LAD, and/or severe 2- or 3-vessel disease) — which in the right clinical context may indicate ACS (Acute Coronary Syndrome).
- Subendocardial Ischemia from another Cause (ie, sustained tachyarrhythmia; shock/profound hypotension; GI bleeding; anemia; etc.).
- ST depression attains up to 5 mm in several leads!
- A comparable amount of reciprocal ST elevation is seen in lead aVR.
- As is seen in ECG #1 — a lesser amount of ST elevation is sometimes seen in lead V1.
 |
| Figure-1: The initial ECG in this case, done in the field by the EMS team (See text). |
- The case I presented in My Comment to that March 9, 2020 post showed a patient with this pattern — who on cath had no more than minimal coronary disease.
- Dr. Smith also referenced an article by Knotts et al, showing that even when diffuse subendocardial ischemia is due to coronary disease — that only a minority of patients had severe LMain coronary disease as the cause.
Sent by anonymous, written by Pendell Meyers
A man in his late 40s presented to the ED with concern for allergic reaction after accidentally eating a potential allergen, then developing an itchy full body rash and diarrhea. In the ED he received methylprednisolone, diphenhydramine, and epinephrine for possible anaphylaxis. Shortly after receiving epinephrine, the patient developed new leg cramps and chest pain. The chest pain was described as sharp and radiated to both arms.
During active chest pain an ECG was recorded:
Meyers ECG interpretation: Sinus tachycardia, normal QRS complex, STD in V2-V6, I, II, III and aVF. Reciprocal STE in aVR, and a touch in V1 (closest lead to aVR). The precordial STD persists in severity from V4-V6, rather than being maximal in V1-V4 (as in posterior OMI), and so the ECG overall best fits the subendocardial ischemia pattern (diffuse supply/demand mismatch). This pattern occurs regardless of whether the cause is ACS (decreased supply) or any other cause of decreased supply or increased demand. There is a tiny hint of STE in aVL, but overall I do not think this looks like high lateral OMI.
A "STEMI alert" was called and soon cancelled. His vitals are unfortunately unavailable during the chest pain episode.
Pain lasted for approximately 45 minutes.
Initial high sensitivity troponin I returned within normal limits at 10 ng/L (less than 20 is reference range for men for this assay).
After pain had resolved, another ECG was performed:
 |
| Almost resolved compared to ECG above. |
Given the ECG changes, he was admitted for further workup.
Repeat troponins were:
94 ng/L
190 ng/L
(none further were ordered)
Formal cardiac echo showed:
EF 73%, normal systolic and diastolic function, normal LV cavity size and wall thickness
No valvular stenosis of regurgitation
Coronary CT Angiogram:
Mid LAD with less than 25% stenosis
All other arteries with no noted stenosis of plaque
Interpreted as "mild, nonobstructive coronary atherosclerosis"
The patient was discharged.
It is unclear to me whether this case could represent 1) simple supply/demand mismatch due to increased demand from epinephrine, 2) Kounis syndrome (usually described as mast cell mediated coronary vasospasm during allergic reaction), 3) brief autolysed left main or LAD ACS with no findings on later echo and CT coronary angio, or 4) something else.
Learning Points:
You must learn and recognize the ECG patterns of OMI and subendocardial ischemia to best understand the ECG in acute care medicine.
Subendocardial ischemia manifests as diffuse ST depression in downward and leftward leads, with maximal precordial STD in V5-V6 and lead II, and reciprocal STE in aVR. You must understand that this pattern does not differentiate ACS from other causes of supply/demand mismatch.

No comments:
Post a Comment