CASE — This ECG was posted by David Richley on the ECGs & Cardiology Fans site on 9/15/2015.
- Unfortunately, there was no history (we don't even know the age of the patient ...) — but it makes for a very interesting discussion. Spurred by a flurry of 1-line answers (predominantly in favor of SVT as the answer) — I added the Comment below.
 |
| Figure-1: Original ECG posted on ECGs & Cardiology Fans. |
Interesting case. In the hope of making a constructive and educational comment — I will suggest that EVERYONE so far has given a suboptimal answer … Perhaps the BEST constructive feedback I can offer is that the MINDSET should be CHANGED with how you answer this question!
It is a GREAT case! It would be nice to know the history (and the age of the patient) — but sometimes you don’t, and we need to deal with this …
The MINDSET that I suggest you strongly consider adapting is that there are 3 (not 2) possible answers !!!! These answers are: i) that you KNOW this is an SVT rhythm; ii) that you KNOW this is VT; or iii) that you are NOT certain what the rhythm is (SVT or VT) — in which case you can then provide a “relative likelihood” as to which you think it is. This is “real life” — because often we will NOT be certain what a rhythm is at the time we need to treat it — AND, it is OK not know for certain. I fully acknowledge that I am not 100% certain as to what this rhythm is based on this single rhythm strip. That’s fine — because the rhythm clearly needs to be treated NOW, and if on the scene I’d know hemodynamic status and would then know how to act accordingly.
In my opinion — an OPTIMAL ANSWER to this tracing is to state what we DO know — which is that there is a regular, slightly widened QRS rhythm at ~ 210-220/minute without clear evidence of sinus P waves. FAR BETTER than to randomly guess “SVT” or “VT” — is to DESCRIBE what you see. Here, you see a regular WCT ( = Wide-Complex Tachycardia) without sinus P waves.This should take no more than 5 seconds to establish ...
Starting from this premise — We need to remember the STATISTICS — which are that in > 80% of cases, a regular WCT without sinus P waves is VT. So even BEFORE you look at the actual ECG — if told you have a regular WCT without sinus P waves, you should GUESS VT — and you’ll be right >80% of the time! If the patient is “older” (perhaps anything over 50 or so) AND has underlying heart disease — you are already up to ≥90% of regular WCT rhythms without sinus P waves being VT. Those are pretty good odds. In view of these odds — your mindset SHOULD BE that the burden of proof is to prove this is SVT and NOT the other way around. Instead, assume VT and treat accordingly. That doesn’t necessarily mean you need to shock the patient (if they are hemodynamically stable) — and I would NOT necessarily shock this patient … — but you need to be coming from the mindset that this is VT until you prove otherwise.
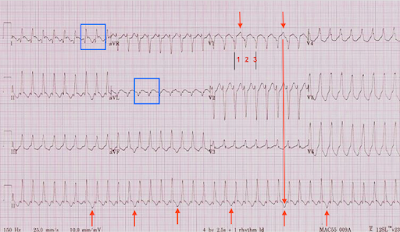 |
| Figure-2: Labeled tracing (See text). |
The rate is ~ 210-220/minute (NOT ~250/minute!). When the rhythm is fast and regular — the EASY way to accurately estimate rate is by the Every-other-Beat method. I pick a QRS that begins or ends on a heavy line (See my vertical BLACK lines in V1) — and then measure the R-R interval of every other beat ( = half the rate). The R-R interval of every-other-beat is just less than 3 large boxes — so half the rate is a little faster than 300/3 or ~ 105-110/minute) — so the actual rate is TWICE that or ~ 210-220/minute. This is relevant, since a rate of 210-220/minute is perfectly within the range for VT — and it virtually excludes AFlutter from consideration (too fast for 2:1 flutter).
I review my approach to distinguishing between SVT vs VT in my ECG Blog #42 — http://ecg-interpretation.blogspot.com/2012/05/ecg-interpretation-review-42-vt-brugada.html —
My thoughts on this tracing are that QRS morphology in the chest looks consistent with LBBB, because the QRS is negative in lead V1 and all upright in lead V6. The axis is directed inferiorly (probably ~ +75 degrees, judging from QRS amplitudes in the limb leads) — so the combination of LBBB-like appearance in chest leads (implying RV origin) and inferior axis (implying the impulse starts from the top = base of the heart, and heads south) = RV OT VT ( = Right Ventricular Outflow Track VT) until proven otherwise.
So WHY isn’t this aberrantly conducted VT? There are several reasons I think this is unlikely: i) Statistics (>80% pre-ECG probability as I describe above); ii) Aberrant conduction should ideally manifest a QRS morphology that looks like some form of conduction defect — and this tracing does NOT. With typical LBBB — you just don’t get such rapid progression from the all negative QRS in V1 to already all positive by lead V3 ….); and iii) I think there is AV Dissociation …
When you see AV Dissociation — it PROVES VT. That said, it is rare in my experience that one can be 100% certain of seeing AV dissociation in most cases of WCT when the rate is fast. I think this is an exception — as RED arrows in V1 highlight what clearly looks like independent P waves in V1. Dropping a vertical line down to the long lead II rhythm strip suggests we DO periodically (albeit not completely at a regular R-R interval) see this deeper-than-expected dip in the ST segment. But I’m not certain of this …
Finally — there looks to be ST segment elevation in at least 2 leads (within the BLUE rectangle). It is really lead I that caught my eye, as the coved shape to the elevate ST segment with associated Q wave in this lead looks REAL. And of course a common clinical setting for sustained VT is acute MI, so perhaps that is what is going on.
BOTTOM LINE: I am not certain what this regular WCT rhythm at ~ 210-220/minute without sinus P waves is …. but my hunch (with my estimate of >90% likelihood) is that it is VT. If the clinical setting was an adult of a certain age with chest pain — then I’d strongly suspect associated acute STEMI and cardiovert. If on the other hand, there was no clinical suggestion of acute MI and the patient was young and totally stable — then I’d probably start with adenosine given likely RVOT VT that may respond to adenosine. “Ya gotta be there” to know what one would do clinically.
I wonder what David Richley thinks?

No comments:
Post a Comment